What can a Psychotherapist not do?
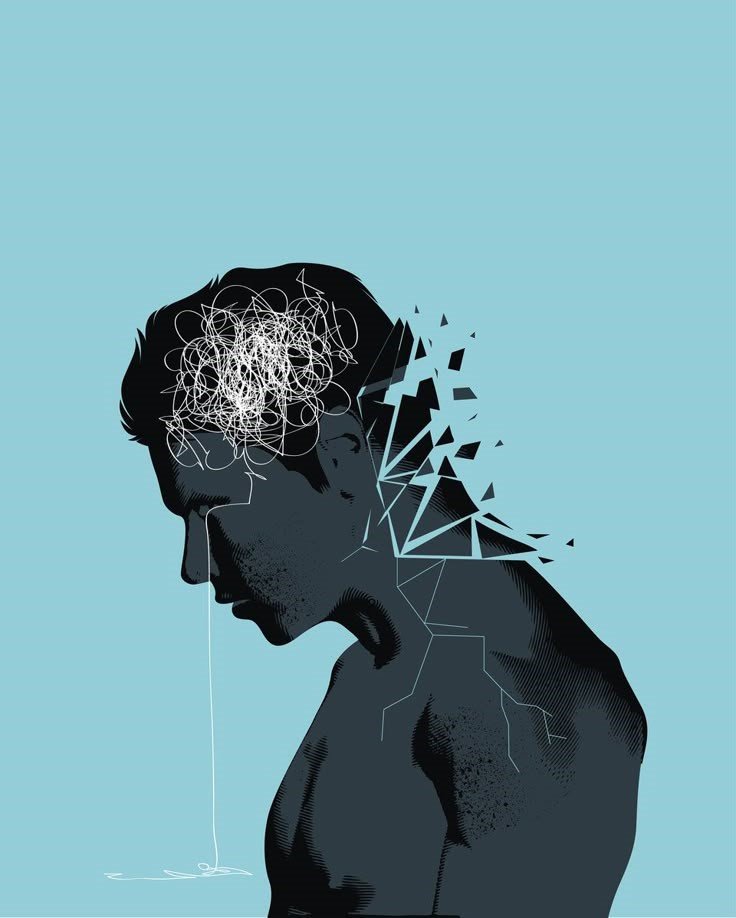
When most people think of psychotherapy, they imagine a safe space where they can share their deepest thoughts without judgment. But many wonder, what can a psychotherapist not do? Understanding psychotherapist boundaries is essential,not just for setting realistic expectations but for protecting yourself and ensuring therapy works for you. Therapists are trained to guide, support, and listen, but they cannot break confidentiality, give direct advice like a life coach, or act as your friend. Knowing these ethical rules for therapists helps clients spot therapist red flags and understand psychotherapy limitations.
I remember a client who came to me, frustrated because their previous therapist seemed more like a friend than a professional. They expected life advice and constant reassurance, and when that didn’t happen, they felt abandoned. Situations like these highlight the importance of clear boundaries in therapy, so you can truly heal-thrive.

Problem Identification
Most people begin therapy believing a therapist can do everything, fix emotions, give the right answers, or even “save” them from their past. But here’s the truth many don’t hear before starting psychotherapy: a therapist is a guide, not a savior.
Understanding what therapists cannot do is just as important as knowing what they can do. When clients expect therapists to act like friends, life coaches, or miracle-workers, therapy becomes confusing, disappointing, and sometimes harmful.
I’ve heard stories, too many, honestly, of clients who left therapy feeling worse, not because therapy doesn’t work, but because boundaries were unclear.
- A therapist who shares too much about their personal life
- A therapist who tries to “fix” you instead of supporting your growth
- A therapist who pressures you to talk before you’re ready
- Someone who acts like they are the only person who understands you
These are concerning concerns. Therapy is meant to include structure, ethics and emotional safety. When those boundaries are crossed, trust is broken.
Research has consistently, through various studies found that the therapeutic relationship is the key mechanism of change (Gelso & Silberberg, 2016; Goldfried, 2013) to the therapeutic process, not advice-giving or “quick fixes”. Trust, ethical practice and boundary-setting are all crucial in developing a strong therapeutic relationship. Therapy is powerful but it is not magic, nor is the therapist meant to be a guru. As a psychotherapist, I am meant to be a skilled partner in your healing process, you are the one who will become aware and develop the resilience and emotional tools to sustain positive change. And that is why there are lines that should never be crossed.
What Psychotherapists Cannot Do
1. A Psychotherapist Cannot Break Confidentiality
(Unless there is risk of harm or legal obligation)
Let me be very direct here: confidentiality is sacred in psychotherapy.
Your therapist cannot share your information with friends, family, or anyone else, not even out of “concern” or “curiosity.”
The only exceptions?
- If you are in immediate danger
- If someone else is in danger
- Court-ordered disclosure
- Mandatory reporting (child or elder abuse)

One time, a client came to me terrified because their previous therapist casually mentioned something personal to a family member. Their trust in therapy was shattered. And honestly… it took months to rebuild their sense of safety.
Confidentiality isn’t optional, it’s the foundation of healing.
2. A Psychotherapist Cannot Give Direct Life Advice
(Therapy is not life coaching)
Sometimes clients ask, “Just tell me what to do!”
Believe me, I get it. We all want clarity.
But psychotherapy isn’t about giving orders, it’s about helping you discover your own clarity and strength (Goldfried, 2013).
Telling you “break up with them” or “quit your job” isn’t ethical and isn’t therapy.
A former client once said their previous therapist constantly gave instructions. When things didn’t go well, they felt guilty and dependent, almost like they had no inner compass.
Good therapy builds self-trust, not obedience.
3. A Psychotherapist Cannot Be Your Friend, Date You, or Do Business With You
Let’s say it clearly:
No friendships. No dating. No business deals. No “hanging out.”
Dual relationships blur judgment and harm clients (Christensen & Jacobson, 1994).
I once worked with someone who said their former therapist started texting casually, joking, and inviting personal conversations. Eventually, the client felt emotionally confused and dependent.
Therapy must remain a professional, safe container.
Anything else crosses the line.
4. A Psychotherapist Cannot Prescribe Medication
(Unless they’re also a psychiatrist or licensed prescriber)
This is one of the biggest misconceptions, Most therapists cannot prescribe medication.
Only psychiatrists, psychiatric nurse practitioners, or certain licensed medical doctors can prescribe.
A client once felt frustrated because their therapist kept saying “you might need medication,” but couldn’t help them get it. No coordination. No support.
Therapy should guide you toward resources, not leave you hanging.
5. A Psychotherapist Cannot Judge, Shame, or Criticize You
Therapy is not a place for judgment.
If your therapist rolls their eyes, shames you, or treats you like you’re “broken,” that’s not therapy , that’s harm.
I once supported a client who felt terrified to speak in therapy because their previous therapist constantly questioned their reactions like:
“Why would you do that? That makes no sense.”
That client carried shame for months.
Healing happens when we are seen with dignity, respect, and compassion, not criticism.
A therapist’s role is to understand , not to shame you into change.
6. A Psychotherapist Cannot Run Directionless, Endless Therapy
Good therapy has structure, even if it’s gentle and flexible.
Your therapist cannot simply sit silently for months while you spiral.
Research by Markowitz & Milrod (2015) shows that when therapy lacks direction, clients often get stuck , not better.
A client once told me they saw a therapist for over a year who just nodded and said, “How does that make you feel?”
No goals. No roadmap. No movement.
Therapy is not meant to be emotional circling , it’s a collaboration toward growth.
7. A Psychotherapist Cannot Forget Who You Are
Therapy is personal.
If a therapist repeatedly forgets your story, your trauma, your progress , that’s a sign of detachment or overload.
Of course, therapists are human. But if every week feels like starting from zero?
Something’s wrong.
A client once told me:
“Every session felt like she was meeting me for the first time… I didn’t feel seen.”
The therapeutic relationship is built on memory, presence, and connection.
8. A Psychotherapist Cannot Ignore You, Yawn Through Sessions, or Scroll Their Phone
This shouldn’t have to be said… but sadly, it does.
A therapist cannot:
- Text or scroll
- Yawn constantly from boredom
- Emotionally disconnect
- Look irritated or “checked out”
I once worked with someone whose past therapist literally yawned loudly during emotional moments.
Do you know what message that sends?
“You don’t matter.”
Therapy requires active presence and attunement , not passive sitting.
9. A Psychotherapist Cannot Pressure You to Stay in Therapy
(No “I’m the only one who understands you” behavior)
Therapy should never feel like emotional captivity.
If a therapist implies or says:
- “You won’t get better without me.”
- “I’m the only one who truly understands you.”
- “Leaving therapy means you’re giving up.”
That’s not care , that’s control.
A client once shared that their previous therapist guilt-tripped them every time they mentioned taking a break. They weren’t healing , they were staying out of fear.
Healthy therapy empowers you to stand on your own ,not depend forever.
10. A Psychotherapist Cannot Work Outside Their Expertise
No therapist can treat everything , and no ethical therapist pretends to.
For example, a trauma therapist may not be trained in eating disorders, and a couples therapist may not be the right fit for severe OCD.
A client once told me their previous therapist tried to treat panic attacks without any training , offering vague advice like “just breathe through it.”
It didn’t help , it made things worse.
True professionalism means knowing your limits and referring when needed.
11. A Psychotherapist Cannot Guarantee Results
(No “You’ll be healed in 6 sessions” promises)
Therapy is not a miracle product , it’s a process.
No honest therapist will say:
- “You’ll be cured in 2 months.”
- “I guarantee success.”
Psychotherapy research (Garfield, 1983) shows outcomes vary by:
- Commitment
- Environment
- Personal pace
- The therapeutic relationship
A client once came to me frustrated , their former therapist promised fast results. When that didn’t happen, they felt broken , like failure was their fault.
You don’t “fail” therapy.
Therapy adapts to you.
12. A Psychotherapist Cannot Force You to Talk About Trauma
Therapists help you process trauma , not push you into it before you’re ready.
You set the pace.
You choose the timing.
Healing cannot be rushed.
I once met a client whose previous therapist insisted on “digging deep” from session one. The client shut down, stopped going to therapy, and avoided emotional conversations for months.
Trauma work requires safety, pacing, and consent , not pressure.
13. A Psychotherapist Cannot “Fix” You
(Because you are not broken)
Therapists don’t “repair” people , they support growth, awareness, and self-leadership.
You don’t come to therapy because you’re broken.
You come because you’re human , with emotions, history, and complexity.
A client once told me they felt “defective” because a previous therapist treated them like a problem to solve.
We spent months rebuilding self-worth, not because they were broken , but because they deserved to see their own wholeness.
Good therapy says:
“You’re capable , let’s expand your capacity.”
14. A Psychotherapist Cannot Become Your Parent or Partner
(Healthy support ≠ emotional replacing)
Therapists hold space , they don’t replace:
- parents
- friends
- partners
- community
Therapy is connection, but not substitution.
A young adult once shared that their therapist became the only person they trusted , to the point they stopped forming new relationships.
Healing included building real-world social muscles, not just bonding in the therapy room.
Therapy strengthens your life outside the office , not replaces it.
15. A Psychotherapist Cannot Decide Your Life Path
(No “You should break up,” “quit your job,” “cut them off” commands)
A therapist can help you clarify.
Support your thinking.
Explore your fears.
Understand your values.
But they cannot direct your life like a GPS.
A client once said they felt pressured by a previous therapist to quit a job immediately for mental-health reasons , without considering financial or emotional factors.
Instead of clarity, they ended up in crisis.
Guidance ≠ instructions
Therapy builds self-trust, not dependency on expert orders.

So… What DOES a Good Psychotherapist Actually Do?
(Beyond the limitations , here’s the truth about ethical, effective therapy)
A therapist’s job isn’t to control you, judge you, or “fix” you , It is to help you:
- Understand yourself deeply
- Build emotional and cognitive skills
- Heal past wounds safely
- Strengthen your nervous system and executive functioning
- Live a life aligned with your values
- Become your own guide over time
Great psychotherapy is collaborative, empowering, research-informed, and deeply human.
As Gelso & Silberberg (2016) emphasize, the therapeutic relationship is not about authority ,
it’s about a real, authentic human connection that supports growth.
And as Goldfried (2013) notes, psychotherapy works when both client and therapist actively engage in clear, goal-oriented change , not passive talking sessions.
Real Therapy Isn’t “Talking Forever” — It Builds Skills
At Heal-Thrive, sessions include:
- Emotional regulation tools
- Executive functioning training
- Trauma-informed resilience building
- Nervous system stabilization
- Practical life strategies
- Values-based decision-making exercises
We don’t just explore your past. We strengthen your present and future.
Therapy should feel like:
“I am growing. I am learning. My life is becoming more mine.”
Not like:
“I sit here and vent and nothing changes.”
How to Recognize a Good Therapist (Green Flags)
(What healthy, ethical, effective therapy looks like)
Not all therapy is the same , and not all therapists practice with the same ethics, emotional intelligence, or skill.
A good psychotherapist:
Green Flag | What It Means | Why It Matters |
Sets clear boundaries | You know the rules, roles, expectations | Safety & predictability = healing environment |
Builds a collaborative plan | Therapy goals are created with you | You stay empowered, not passive |
Checks in about your progress | “How is this working for you?” | Adjusts treatment — not one-size-fits-all |
Values cultural & identity awareness | Your background and identity matter | You feel seen, not erased |
Holds space without judgment | You can show all parts of yourself | Shame has no room in healing |
Uses research-informed methods | CBT, ACT, trauma-informed, EF coaching, etc. | Your healing is structured, not random |
Encourages emotional regulation | Breathwork, grounding, nervous-system tools | Healing happens in the body too |
Teaches executive function skills | Scheduling, planning, self-management | Emotional health & functioning connect |
Supports independence | Goal: you don’t need therapy forever | Growth over dependency |
Welcomes feedback | You can say “this isn’t working” | Trust becomes mutual, not one-sided |
Good therapy is not about perfection.
It’s about presence, ethics, structure, science, and humanity.
As Garfield (1983) wisely noted:
“Psychotherapy works , but it’s a process of mutual work, not magic.”
Short Real-World Client Example
A client once came in saying:
“I feel like my last therapist just listened. I didn’t grow.”
At Heal-Thrive, we rebuilt the process:
- Clear goals
- Trauma-aware relational work
- Executive skills training
- Nervous-system grounding
- Values-based life strategies
In six months:
- Anxiety reduced
- Self-trust increased
- Daily routines stabilized
- Relationships improved
Because healing isn’t passive . It’s active collaboration.
When It’s Time to Switch Therapists (Major Red Flags You Should Never Ignore)
Recognizing unsafe, ineffective, or unethical therapy
Sometimes therapy doesn’t feel right , not because you are resistant to growth, but because the therapist isn’t holding an ethical, supportive, or effective space.

And yes… switching therapists can feel scary.
You may think:
“What if the problem is me?”
“I don’t want to hurt their feelings.”
“They know so much about me , starting over is exhausting.”
Trust me, these feelings are normal.
But good therapy should not feel confusing, boundary-blurry, or unsafe.
A healthy therapist supports your independence ,not dependence, guilt, or discomfort.
Reminder: A therapist is not allowed to be your friend, savior, parent, or moral judge.
Their role is professional , supportive, human, caring, but professional.
Client Story: When a Therapist Crossed a Line
I once worked with a client who left a therapist because:
- They texted late-night emotional messages,
- Shared personal marriage problems,
- And suggested meeting “as friends” outside sessions.
The client felt guilty leaving, but secretly anxious every week.
Within months of working together safely:
- Their sleep improved
- Anxiety reduced
- They rebuilt confidence in boundaries
- They finally felt emotionally safe
Leaving the wrong therapist is not quitting therapy. It’s protecting your mental health.
Healthy Therapy vs. Unhealthy Therapy (Quick Comparison)
Healthy Therapy | Unhealthy Therapy |
Empowering | Controlling / dependent |
Collaborative goals | No goals, vague |
Professional boundaries | Personal / romantic blur |
Validates your experience | Dismisses feelings |
Encourages autonomy | Creates neediness |
Uses evidence-based methods | Personal opinions only |
Welcomes feedback | Defensive or offended |
If you’re unsure, ask yourself:
Do I feel safe, respected, and seen?
If the answer isn’t yes, you deserve better.
If you’re thinking of switching therapists…
You aren’t failing.
You are choosing your mental health.
And that is strength.
The Ethical & Legal Rules Psychotherapists Must Follow
Non-negotiable standards that protect clients in the U.S., especially California
In the U.S. , and particularly in California, where therapist regulations are some of the most rigorous , mental health professionals follow strict laws and ethical standards.
These rules are set by organizations like:
- APA , American Psychological Association
- ACA , American Counseling Association
- NASW , National Association of Social Workers
- California Board of Behavioral Sciences
- HIPAA privacy laws
These standards exist to protect you, your privacy, your emotional safety, and your autonomy.
Core Ethical Standards Every Psychotherapist Must Follow
Rule | What it Means |
Confidentiality | Your information stays private unless specific legal exceptions apply |
Informed Consent | You must be told how therapy works, risks, and your rights |
Competence Only | They must only treat what they are trained for |
Avoid Dual Relationships | They cannot be your friend, partner, boss, landlord, etc. |
No Exploitation | They cannot use you emotionally, financially, or sexually |
Cultural & Identity Respect | They must honor your background & identity |
Professional Boundaries | Time, communication, and emotional limits exist |
Client Autonomy | You make your own choices , not the therapist |
Ongoing Education | Must stay up-to-date with science & ethics |
Careful Record Keeping | Your notes must be secure, accurate, and private |
Duty to Protect | They act to prevent harm if someone is in danger |
A therapist who isn’t following these… isn’t practicing therapy.
They’re breaking the code of ethical healing.
Legal Situations Where Confidentiality CAN Be Broken
(Ethical — not a violation)
Confidentiality can only be broken if:
- You are in danger of harming yourself
- You plan to seriously harm someone else
- A child, elder, or dependent adult is being abused
- Court demands records (in specific legal cases)
These laws aren’t meant to punish.
They exist to protect life and safety.
Anything beyond this? Not allowed.

Mini Case Story: When Ethics Healed Trust
A client once told me:
“I felt uncomfortable because my old therapist shared too much about their life. I didn’t feel safe opening up.”
We rebuilt trust through:
- Clear boundaries
- Transparency about treatment goals
- Trauma-informed emotional safety
- Consistent check-ins on comfort level
Soon, she shared deeper feelings, improved assertiveness, and regained emotional stability.
Boundaries aren’t cold , they create space for authentic connection and client empowerment.
What To Do If Your Therapist Crosses a Boundary
Making the Situation Better:
- Stop & Check in With Yourself
Notice what made you uncomfortable, and explore what you felt.
- Remember What Happened
Write down the time and the behavior and your emotional response.
- Explore Your Needs
Consider whether you would like to talk to your therapist about it or find another therapist.
- Speak Kindly & Respectfully (if that’s an option for you)
You can say:
“When , happened, I felt uncomfortable. Can we talk about boundaries?”
- End Therapy If You Feel That’s Helpful or Necessary
“I think another therapist is a better fit for me, at least for now.”
- Report Abuse or Harm
If you experienced abuse or harm, report it, if you feel comfortable. You can reach out to reporting authorities in California or the U.S.
- Reach Out for Support, and Consider Starting Therapy with Someone New
You can reach out to trusted friends and family for support, or talk to new therapy you have been wanting to try.
Important Reminder
You have the right to:
- Feel safe
- Be respected
- Be heard
- Make your own choices
- Receive support
You deserve a healthy therapeutic space
Frequently Asked Questions — What Therapists Cannot Do
- Can my therapist provide advice like a life coach and simply tell me what to do?
No. Therapists do not give personal or directive advice; they provide support, guidance, and resources but do not tell clients what to do.
- Can a therapist break confidentiality and share my information with others?
Only in limited legal circumstances: including a risk of harm to self or others, abuse of a vulnerable person, or a court order.
- Can a therapist be a friend, or date me?
No, dual relationships are unethical and inconsistent with safe care.
- Can a therapist prescribe medication?
Only if they are a licensed psychiatrist. Most therapists cannot prescribe medications.
- Can a therapist judge or shame me?
No. Therapy must be a safe, non-judgmental space.
- Can a therapist guarantee results?
No. Therapy outcomes vary; it’s a process, not a promise.
- Can a therapist force me to talk about trauma?
No. You control the pace and timing of trauma discussions.
- Can a therapist work outside their area of expertise?
No. Ethical therapists treat only what they are trained for and refer when needed.
- Can a therapist ignore boundaries or be inattentive?
No. Active presence, professionalism, and respect for your time are mandatory.
Take the Next Step Toward Healing
You deserve therapy that is:
- Safe
- Respectful
- Professional
- Supportive
If you’ve ever felt unsure, judged, or unsafe in therapy, it’s okay to switch. Healing is about your personal discovery, rather than what someone else imposes on you.
At Heal-Thrive, we work with clients to:
- support you in understanding yourself and your needs.
- navigate ethical and safe therapy, everything within your boundaries.
- build executive function, emotional resilience, and trauma-informed coping strategies.
- establish clear goals while providing/using actionable steps.
Next Steps:
- Contact a Certified Therapist – Set up a consultation, and feel free to ask about boundaries and methodology.
- Download Our Free Guide – “How to Choose a Therapist You Can Trust.”
- Book A Session Today – Don’t hesitate to embark on a safe and empowering therapy journey.
It’s your right to heal, and you do not have to do it alone.
Client Success Summary Anonymized)
Case 1:
A client left a previous therapist where they felt pressured to engage in conversation about trauma. At Heal-Thrive, in a pace and trauma-informed session:
- Their anxiety levels decreased by 40%
- They experienced an increase in emotional regulation
- Their confidence and autonomy were strengthened
Case 2:
A client came in with ADHD along with executive function issues. They had been in a therapy where there were no tangible goals. At Heal-Thrive:
- Their daily living became increasingly organized
- They began to manage tasks and to-do lists more effectively
- They reported improvements in their self-esteem and sense if independence
Case 3:
Anxiety client felt shamed or dismissed in a previous therapeutic experience, and connected with a therapist that respected boundaries:
- They began to develop trust in the therapeutic process,
- They began to re-establish connections with personal values and desires, and
- They reported connection or mobilization of meaningful change in life
It is important to note that while healing can include fumbling experiences, it is about safe, ethical, and growth-oriented space.