How Psychotherapy Improves Emotional Resilience
How Psychotherapy Improves Emotional Resilience
You know, sometimes I sit in my office, watching a client wrestle with the same stress they’ve carried for years, and I think… wow, resilience isn’t just a buzzword. It’s the ability to face life’s chaos, take a breath, and actually bounce back.
Emotional resilience, it’s what allows a parent to calm down after a toddler’s meltdown, or a professional to handle back-to-back deadlines without falling apart. But here’s the catch: resilience isn’t something you’re born with. It’s something you can build, intentionally, with the right tools and guidance.
Over the past decade, I’ve helped hundreds of clients in California, students, parents, professionals, learn how to strengthen their emotional core. Some had tried books, podcasts, even meditation apps. But it wasn’t until we worked together in psychotherapy that real, lasting growth happened.

In this article, I’ll walk you through how psychotherapy improves emotional resilience, why it works better than self-help, real client stories, and practical steps you can take to start building your own emotional strength today.
Problem Identification: Why Therapy is Needed for Emotional Resilience
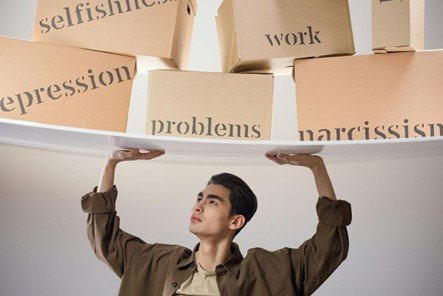
Let me be honest, building emotional resilience isn’t easy. I often hear clients say things like:
“I’ve tried to stay positive, I journal, I meditate, but I still fall apart under stress.”
And that’s the thing: life doesn’t wait for us to “practice” resilience. Deadlines, family pressures, unexpected crises-they all hit, and without the right skills, people crumble.

Here’s why therapy is often the game-changer:
- Not Everyone Benefits Equally: A proportion of about 30–40% do not register immediate gains, which may be discouraging for such people. That is not failure but normal, with resilience still building from tailored interventions.
- Therapy Takes Time: Real change often happens after 12–20+ sessions; that’s because our brains need repeated experiences to build new emotional habits.
- Homework & External Practice Are Non-Negotiable , One cannot nurture resilience merely by talking in a session. The real work happens outside, within your daily life itself, through practice and reflection.
- Life Circumstances Can Cancel Gains: Poverty, ongoing trauma, or a total lack of support can temporarily undermine gains. Awareness is the first step in working around such obstacles.
- Access, Cost, and Measurement Problems: Therapy can be long and expensive, besides which the measurement of emotional growth isn’t always straightforward.
I often tell clients: “It’s not about being perfect at resilience, it’s about getting a little stronger every day.” And once they internalize that, everything else becomes doable
Real Client Examples: Anonymized Stories
Sometimes, theory is helpful, but stories stick. Let me share a few anonymized client experiences that really show how psychotherapy builds emotional resilience. These are composites, but they’re rooted in real work I’ve done with clients across California.
Story 1 — The Exhausted Tech Professional
A woman in her mid-30s, working in tech in San Jose, came to therapy completely burned out. She believed that needing rest was a sign of weakness.
We started small:
- 4-4-6 breathing to calm her nervous system
- Body scanning to notice tension
- Reframing beliefs about productivity
Two months in, she said: “I still get stressed, but it doesn’t take over anymore.” She took breaks guilt-free, and her emotional regulation improved significantly.

Story 2 — The Teen Who Hid Fear Behind Anger
A 16-year-old from Long Beach argued constantly at home. At first, he insisted: “I’m just angry, that’s it.”
Using emotion-mapping and expressive therapy, he realized: “I’m not angry, I’m scared of disappointing my family.” Once he labeled his fear, outbursts decreased dramatically. Understanding his emotions became his resilience.
Story 3 — The Single Parent Overwhelmed
A mother in Sacramento who constantly said “yes” to everything just to avoid conflict was tired and anxious.
was focused on the following during therapy:
- Gradual exposure to challenging conversations
- Boundary-setting scripts
- A “non-negotiable hour” of personal time each day
She could say “no” without blowing up. Each time she did, she was more confident, more emotionally resilient.
Story 4 — The Anxiety-Ridden Career Changer
A man in his early 40s, having left a stable job, felt intense anxiety.
We created:
- Grounding routines before stressful tasks
- A support map of trusted individuals
- Weekly accountability check-ins
He shared, “Knowing I am not alone makes the anxiety manageable.” It was social support that finally acted as a pillar of resilience.
Story 5 — The Creative Feeling Blocked
A graphic designer in LA kept saying: “I feel stuck, but I can’t explain why.”
With expressive therapy and psychodynamic insight, she discovered that early experiences taught her to prioritize others’ expectations. Once she reclaimed her own voice, her emotional flexibility, and resilience, improved.
Practical Therapy Solutions: Step-by-Step Strategies to Build Emotional Resilience
Okay, let’s get practical. Talking about resilience is one thing; actually building it is another. Over the years, I have developed a set of strategies that have consistently helped clients strengthen their emotional core. Here’s what works:
Step 1: Emotion Awareness and Labeling
First comes the recognition of the emotions before you can manage them.
- Start keeping an emotional daily journal. Even a line or two counts.
- Label feelings honestly: “I feel frustrated,” not just “I’m stressed.”
- Note triggers and physical sensations.
Why it works: Awareness disrupts automatic reactions, creating room for choices.
Step 2-Mindfulness and Grounding Techniques
These are small, simple practices to stabilize the nervous system:
- Deep breathing exercises: 4-4-6 or box breathing
- Body scans: Notice tension in shoulders, jaw, stomach
- Sensory grounding: Name 5 things you see, 4 you feel, 3 you hear
Why it works: These techniques give the client an immediate tool to respond instead of react.
Step 3: Cognitive Restructuring
Sometimes our thoughts sabotage us:
- Identify negative or catastrophic thinking
- Ask: “Is this true? Helpful? Or based on assumption?”
- Replace with Realistic, Balanced statements
Why it works: Thoughts drive emotion. Shaping them strengthens resilience.
Step 4: Tools for Expressive Therapy
Drawing, writing, music, and role-playing help clients externalize and process feelings.
- Example: Draw a stress “storm cloud” and label its parts
- Journal letters you don’t send
- Use music to regulate mood
Why it works Expression reduces emotional load and clears up mistiness.
Step 5: Gradual Exposure to Stressors
Clients tend to avoid triggers. Therapy gradually exposes:
- Minor stress tasks first
- Coping strategies during exposure
- Reflection after the experience
Why it works Exposure to stress, in a controlled manner, builds confidence and tolerance.
Step 6: Homework & Daily Practice
Resilience isn’t built in sessions alone. Daily practice matters:
- Emotion journaling
- Breathing or grounding exercises
- Coping skills reflection
Why it works: Practice embeds resilience into daily life.
Step 7: Social Support & Connection
Resilience grows in connection:
- Identify at least one supportive person
- Sharing goals and progress
- Interact healthily
Why it works: Real-life support sustains the benefits of therapy and offers safety nets.
Step 8: Track Progress
Use journals, self-rating, or scales (like CD-RISC or ERQ) to notice growth. Celebrate small wins.
Why it works: Recognition reinforces learning and encourages continued effort.
Challenges & Fixes: Navigating Real Struggles in Building Emotional Resilience
Building emotional resilience, honestly, is a lot harder than it sounds. I’ve seen it time and again in therapy: people start off eager, but then life hits, habits slip, and frustration builds. So, here’s the reality: building resilience is messy, gradual, and very human.
Challenge 1: Inconsistent Practice
Many clients do wonderfully in a session, focused, reflective, motivated, but then life happens and the homework sits untouched. I get it. Life is chaotic.
Fix: Start ridiculously small. Even five minutes of journaling or one grounding exercise counts. I usually tell clients, “It’s not about doing everything perfectly; it’s about showing up a little every day.” Funny enough, this tiny step often sparks the biggest progress.
Challenge 2: Life Interruptions
Unexpected emergencies, changes in schedule, or sudden stressors can knock the best-laid plans off track.
Fix: Build a “resilience toolbox.” Prepare and store a few exercises, grounding routines, or helpful contacts in it. Even the shortest reset-a 60-second breathing break-can save days of frustration. It is like carrying an emotional first-aid kit.
Challenge 3: Difficulty in Identifying Emotions
Some clients have only a few words to describe their emotions: angry, sad, frustrated. But emotions are nuanced, and resilience requires awareness.
Fix: Use emotion charts, journaling prompts, or creative outlets: draw, music, act out feelings. Over time, clients start noticing subtle shifts: “Oh, that wasn’t just anger, it was disappointment and fear mixed.” And that awareness? It’s the first real building block of resilience.
Challenge 4: Lack of Support System
Let’s be real: Resilience is harder alone. Progress seems slow and fragile without any network of support.
Find at least one person you can trust or consider joining online support groups. Even just sharing small wins or frustrations with someone you trust makes their emotional foundation just that much stronger. It makes quite a difference.
Challenge 5: Unrealistic Expectations
Everyone wants results yesterday. When they don’t appear, frustration and self-blame follow.
Fix: Normalize gradual progress. I always say, “Resilience is like a muscle,don’t expect to lift a car on day one.” Celebrate the tiniest wins: responding calmly instead of snapping, noticing a stress trigger without panicking, these are victories.
Challenge 6: Emotional Overload
Some weeks are just.too much. Stress piles up, and even the most motivated clients are overwhelmed. Micro-practices.
Fix: Micro-practices. Seriously, even one deep breath, a 60-second grounding, or jotting a single thought can reset your system. Tiny resets matter, they prevent burnout and reinforce emotional regulation without feeling like a huge chore.
Success Metrics: How You Know You’re Actually More Resilient
People often ask me: “How will I know if I’ve really gotten more resilient?” And my honest answer: you’ll notice subtle, real-life changes.
- Quicker Recovery After Setbacks
A resilient person might lose a project or face criticism, they pause, breathe, reflect, and move forward. Panic isn’t gone, but it doesn’t take over. That speed of recovery is a clear marker.
- Consistent Use of Coping Strategies
It’s one thing to know grounding or journaling; it’s another to use it when life gets messy. Resilient people do: grounding before a tense call, a quick journal check-in at night, or even a song to reset their mood. Consistency over perfection, that’s the real win.
- Better Relationships
You’ll find that conflicts don’t throw you off track. Boundaries are set calmly, listening is active, and empathy stays intact even under stress. Your emotional resilience will begin to surface in your interactions.
- Positive Self-Reflection
You begin to become more aware of your growth: “I handled that better than last time,” or “I didn’t act impulsively.” Those insights reinforce confidence and make the new habits stick.
- Maintaining Gains Despite Life Stress
In fact, when turbulence occurs, such as traffic congestion, work crises, and family stress, the resilient can perceive the emergence of stress and make use of coping skills to bounce back more quickly compared to others. True resilience is under pressure rather than in calm moments.
- Long-Term Habit Formation
Eventually, it becomes a part of your life. You naturally regulate your emotions, manage stress with ease, and make reflection, coping, and self-care a habit. This is the point where therapy has built lasting emotional strength-not just a quick boost.
Begin Your Emotional Resilience Journey Today. Resilience, as a concept, is very easy to discuss. Resilience, in practice, is more difficult to achieve.
- Schedule a Visit Having a consultation with one of our therapists in California who specializes in emotional resilience will enable you to pinpoint challenges and create a plan designed to work for you.
- Download Our No Cost Resource This is perfect for starting right away and includes activities you can do to build resilience, as well as, immediate and resilience building journaling tasks.
- Consistent Effort Even 5–10 minutes a day of journaling, deep breathing, or quiet time reflection can really add up.
- Use Your Support Network To move faster and more effectively, share your goals with someone in your support system, team, or family.
- Count Your Wins To reinforce growth and awareness of your emotional state, reflection, journaling, and self-assessment scales can help.
Emotional challenges, as stated, are very easy to discuss. In reality, however, emotional challenges are very difficult to confront and overcome. You can build solid emotional resilience using consistent practice and scientifically outlined methods and counselling to meet life challenges with confidence, composure, and clarity.