ADHD and Sleep Revenge: Why Nighttime Feels Like Your Only Quiet (and What to Do Instead)
It’s 11 PM. You’re exhausted. Your body is basically screaming at you to go to bed. But instead, you’re scrolling through your phone, reorganizing your bookshelf, or suddenly deciding tonight is the night you’re finally going to learn how to make sourdough bread from scratch.
Sound familiar?
Welcome to revenge bedtime procrastination ADHD style, where the only time your brain feels like it actually belongs to you is when you should be sleeping.
What Is Revenge Bedtime Procrastination (And Why Does It Have Such a Dramatic Name)?
Let’s start with the term itself. “Revenge bedtime procrastination” sounds like something out of a dramatic thriller, right? But it’s actually pretty spot-on.
The concept originated in China, where people with demanding work schedules started staying up late just to reclaim some personal time. It’s not really about being a night owl or being more productive at night (though those can play a role). It’s about taking back control of your time when you feel like the whole day has been stolen from you.
For those of us with ADHD, this hits different. We’re not just dealing with long work hours. We’re dealing with:
- A brain that never quite feels “caught up”
- Days where everyone wants something from us
- Constant task-switching and interruptions
- Decision fatigue from hundreds of micro-choices
- That feeling that we spent all day being productive for everyone else but never got to the stuff we actually wanted to do
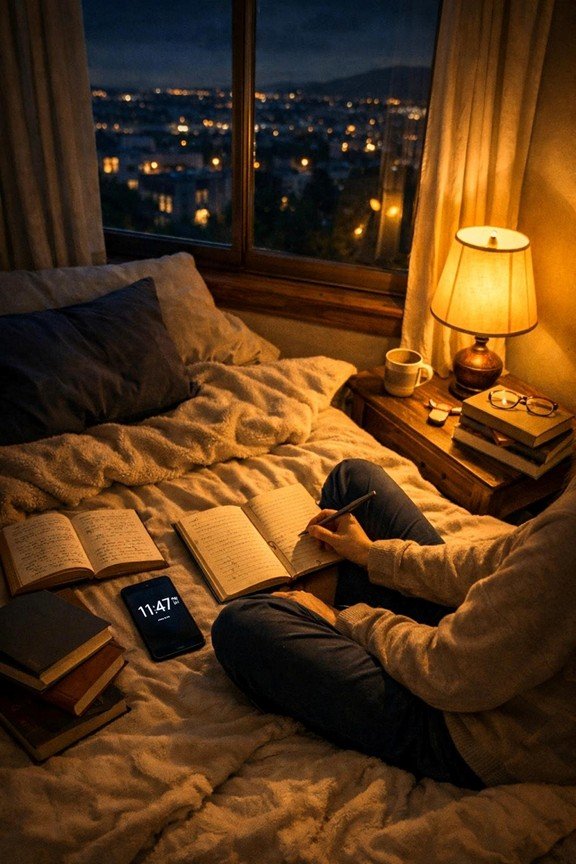
So when nighttime rolls around? That’s when we finally get our time back. That’s when nobody is asking us questions, sending us emails, or expecting us to remember things. The phone stops buzzing. The demands stop coming. And suddenly, staying awake until 2 AM feels less like self-sabotage and more like self-care.
Except… it’s not. And we know it’s not. But we do it anyway.
The Real Reason Nighttime Feels Like Your Only Quiet
Here’s what most sleep advice gets wrong: it treats revenge bedtime procrastation like it’s just bad habits or poor time management. Like if you just tried harder or set better boundaries during the day, you’d magically go to bed on time.
But that’s not what’s happening.
For people with ADHD, nighttime serves three critical psychological needs that aren’t being met during the day:
1. Autonomy: Finally, Nobody Wants Anything From You
During the day, your ADHD brain is constantly being interrupted. Even if you work from home alone, you’re still dealing with notifications, emails, the dog needing to go out, that package delivery, the dentist calling to confirm your appointment, and your brain randomly remembering you never responded to that text from three days ago.
Every interruption costs you. Not just the two minutes it takes to deal with it, but the 15-20 minutes it takes your ADHD brain to get back into whatever you were doing before.
By the time the day is over, you haven’t had a single uninterrupted moment that belonged completely to you. Nighttime becomes the only space where you get to decide what happens next. Nobody is making demands. You’re not “on call” for anyone. And that feeling of autonomy? It’s intoxicating.
This isn’t about being selfish. It’s about finally getting to exist without having to perform, respond, or produce for someone else.
2. Nervous System Regulation: You’re Finally Coming Down
Let’s talk about what your nervous system has been doing all day.
If you have ADHD, your nervous system is likely running hot most of the time. You’re constantly in a state of mild (or not-so-mild) activation because your brain is working overtime to:
- Focus on things that don’t naturally interest you
- Remember tasks and appointments
- Regulate emotions that come in waves
- Filter out distractions and stay on track
- Make decisions about everything from what to eat to which email to respond to first
That’s exhausting. And most of us don’t realize how revved up we are until everything finally stops.
Nighttime is when your nervous system finally gets permission to downregulate. The demands stop. The stimulation decreases. And even though you’re tired, your body is still trying to process and release all that built-up activation from the day.
ADHD sleep delay isn’t just about procrastination, it’s often your nervous system trying to find equilibrium after spending 12+ hours in overdrive.

3. Lack of Boundaries During the Day: You Never Actually Stopped
Here’s the hard truth: many of us with ADHD struggle with boundaries. Not because we don’t want them, but because our brains make it really hard to enforce them.
We say yes when we mean no. We respond to texts immediately even when we don’t have the bandwidth. We keep working past when we said we’d stop because we hyperfocused and lost track of time. We let other people’s urgency become our emergency because rejection sensitivity makes it hard to disappoint people.
By the time nighttime rolls around, we haven’t actually had boundaries all day. We’ve just been available. Responsive. “On.”
So staying up late becomes our way of creating a boundary after the fact. It’s not healthy or sustainable, but it’s the only boundary we feel like we can actually control. Nobody can ask us for anything if they’re all asleep.
Why ADHD Night Productivity Is a Double-Edged Sword
Now, I know what you’re thinking. “But I actually am more productive at night! That’s when I get my best work done!”
And you might be right. A lot of people with ADHD genuinely do experience ADHD night productivity. There are real reasons for this:
- Fewer distractions: The world is quieter, notifications have slowed down, and there’s less sensory input competing for your attention
- Delayed circadian rhythm: Many people with ADHD have a naturally delayed sleep-wake cycle, meaning they’re biologically more alert later in the evening
- Hyperfocus opportunities: With fewer interruptions, it’s easier to drop into that deep focus state that feels impossible during the day
But here’s the catch: even if you can be productive at night, it doesn’t mean this pattern is sustainable or healthy. Sleep deprivation compounds ADHD symptoms in ways that make everything harder:
- Worse executive function
- More emotional dysregulation
- Increased impulsivity
- Poorer working memory
- More difficulty with focus and attention
So you might get stuff done at midnight, but you’re paying for it with interest the next day. And the next. And the cycle continues.
What to Do Instead (That’s Not Just “Go to Bed Earlier”)
Okay, so if the answer isn’t just forcing yourself to go to bed earlier or trying harder to have better sleep hygiene, what actually works?
The key is addressing the root causes: autonomy, nervous system regulation, and boundaries. Here’s how:
Create Protected Time During the Day
If nighttime is appealing because it’s the only time that feels like “yours,” then you need to carve out protected time during the day that serves the same purpose.
This isn’t about productivity. It’s about autonomy.
Set aside 30-60 minutes where:
- You don’t check email or messages
- You’re not “on call” for anyone
- You get to do something purely because you want to
- Nobody can interrupt you
It might be early morning before anyone else is awake, a lunch break where you actually leave your desk, or a specific hour in the afternoon where you’re unavailable. The timing matters less than the consistency and the boundary.
Help Your Nervous System Downregulate Earlier
Instead of waiting until midnight for your nervous system to finally calm down, build in intentional transition time between your “on” hours and your evening.
This isn’t about bubble baths and meditation apps (though if those work for you, great). This is about giving your nervous system what it actually needs:
- Movement: A walk around the block, stretching, dancing to one song
- Sensory regulation: Dim lighting, weighted blankets, calming music, or even just sitting in silence for five minutes
- Brain dumps: Get everything out of your head and onto paper so you’re not trying to remember it all night
- Screen-free time: Even 20 minutes without screens before bed can help signal to your brain that the day is ending
Practice Saying No Earlier in the Day
If part of the revenge is because you spent all day being available to everyone else, start building your “no” muscle during daylight hours.
This is hard. Especially with ADHD and rejection sensitivity. But boundaries during the day mean you won’t feel the need to revenge-reclaim your time at night.
Start small:
- “I’ll get back to you tomorrow on that”
- “I’m not available after 7 PM”
- “I need to think about that before I commit”
- “That doesn’t work for my schedule”
The more you protect your time during the day, the less you’ll feel like you need to steal it back at night.
Reframe Your Relationship With Sleep
Instead of thinking about sleep as the thing that’s stopping you from having your time, try reframing it as the thing that gives you more capacity to have your time well.
Sleep isn’t a waste of your precious hours. It’s the thing that makes those hours actually feel like yours. When you’re well-rested, you have better focus, more energy, and stronger executive function, which means you can actually enjoy and use your time during the day.
When Revenge Becomes a Pattern, Not a Choice
If you’ve read this far and you’re thinking “yeah, but I’ve tried this stuff and I still can’t make myself go to bed,” that’s a sign you might need more support.
Sometimes ADHD sleep delay is about more than just lifestyle changes. It might be:
- Medication timing (if you take stimulants late in the day)
- A co-occurring sleep disorder like delayed sleep phase disorder
- Unaddressed anxiety or depression
- Deep-rooted boundary and autonomy issues that need processing with a therapist
And that’s okay. You’re not broken. You’re just dealing with a brain that works differently, and sometimes that requires professional support.

You Deserve Rest And Autonomy
Here’s what I want you to hear: The need for personal time, autonomy, and a regulated nervous system isn’t selfish or indulgent. It’s human. And the fact that you’re trying to meet those needs: even in ways that aren’t serving you: shows that you’re paying attention to what you need.
The goal isn’t to shame yourself into better sleep habits. It’s to build a life where you don’t feel like you have to wait until everyone is asleep to finally be yourself.
You deserve both rest and freedom. And with the right support and strategies, you can have both.
Ready to Build a Life Where You Don’t Need Revenge?
If revenge bedtime procrastination ADHD patterns are running your life, you don’t have to figure this out alone. At Heal and Thrive Therapy and Coaching, we specialize in helping people with ADHD build sustainable routines, set boundaries, and regulate their nervous systems: without shame or judgment.
Whether you’re looking for ADHD coaching to build practical strategies or therapy to process the deeper patterns keeping you up at night, we’re here to help.
Learn more about our ADHD coaching services or reach out to see how we can support you.
You deserve sleep. And you deserve to feel like your time is your own( long before midnight.)