What is the Best Therapy for ADHD? (Spoiler: It’s Complicated)
What is the Best Therapy for ADHD? (Spoiler: It’s Complicated)
Okay, let’s be real here. If you’ve found yourself googling “best therapy for ADHD” at some ungodly hour with about fifteen tabs open, your brain going a mile a minute, and you’re feeling completely overwhelmed by all the options out there… yeah, I’ve been there. And so have pretty much all of my clients.
I’m an ADHD coach, and I’ve been working with people and families dealing with ADHD for years now. And here’s the thing that might surprise you – there’s no magic bullet. No perfect therapy that works for everyone. I know, I know, that’s probably not what you wanted to hear when you clicked on this post.
But here’s what I can tell you: there ARE therapies that work really, really well. The trick is figuring out which one clicks with how YOUR brain works. Because ADHD is a complex neurological condition that shows up differently in different people, and what helps one person might not do much for another.
Take two of my clients, for example. Jenna’s a college student who came to me because she couldn’t focus on anything for more than five minutes and was constantly forgetting assignments. We did some CBT work together, and it was like a lightbulb went off. She learned to catch those negative thought spirals and actually developed some systems that worked with her brain instead of against it.
Then there’s Mike. He’s a dad with ADHD, and his biggest struggles were more about managing his emotions and not losing his temper with his kids when things got chaotic at home. For him, we focused more on emotional regulation techniques and family dynamics. Completely different approach, but it worked for him.
So in this post, I’m going to walk you through all the different therapy options that actually have research backing them up. I’ll tell you what symptoms each one tends to help with, share some real stories from people I’ve worked with (names changed, obviously), and hopefully help you figure out what might be worth trying for you or your kid.

Because here’s the thing – knowledge really is power when it comes to ADHD. The more you understand what’s out there, the better equipped you’ll be to advocate for yourself and find something that actually makes a difference in your daily life
Let’s Talk About What ADHD Actually Is (And Why Treatment Isn’t One-Size-Fits-All)
Before we dive into all the therapy options, I think it’s important to get on the same page about what we’re dealing with here. ADHD isn’t just “can’t sit still” or “gets distracted easily.” It’s this complex neurological thing that affects how your brain processes information, manages attention, and controls impulses.
And here’s where it gets tricky – ADHD looks different in pretty much everyone who has it. Some people are the classic hyperactive type – they’re bouncing off the walls, interrupting conversations, always fidgeting with something. Others are more the inattentive type – they’re daydreaming, losing things constantly, starting projects but never finishing them. And then you’ve got people who are a mix of both.
But it gets even more complicated than that. ADHD symptoms can change depending on what’s going on in your life. Stress makes everything worse. Not getting enough sleep? Forget about it. Going through a major life change? Your coping strategies might completely fall apart.

I had one client – let’s call her Sarah – who was doing great with her ADHD management for months. She had her systems down, was staying on top of work, feeling pretty good about things. Then she got divorced, and suddenly all her strategies stopped working. We had to completely rebuild her approach because her life circumstances had changed so dramatically.
This is why I always tell people that finding the right therapy for ADHD isn’t a one-and-done thing. It’s more like… okay, this is going to sound cheesy, but it’s like tending a garden. You plant some seeds, see what grows, adjust based on the seasons, maybe try some new varieties. It’s an ongoing process.
The Heavy Hitters: Therapies That Actually Have Science Behind Them
Alright, let’s get into the good stuff. These are the approaches that have been studied extensively and consistently show real results for people with ADHD.
Behavioral Therapy: The Foundation (Especially for Kids)
If you’ve got a kid with ADHD, behavioral therapy is probably going to be one of the first things that gets recommended. And honestly? There’s a good reason for that. This approach is all about changing specific behaviors through consistent feedback and rewards.
Now, I know what some of you might be thinking – “Great, another reward chart.” But it’s actually way more sophisticated than that. Good behavioral therapy teaches both kids and parents how to create structure that works, how to give feedback that actually motivates change, and how to build habits that stick.
I worked with this family – the Johnsons – where their eight-year-old, Emma, was having meltdowns every single morning trying to get ready for school. Mom was stressed, Emma was stressed, everyone was starting the day feeling terrible. Through behavioral therapy, we created this visual routine chart that broke down the morning into tiny, manageable steps. But the real magic happened when we taught Mom how to give Emma specific, positive feedback for each step she completed.
Within about three weeks, mornings went from total chaos to… well, not perfect, but manageable. Emma felt proud of herself, Mom wasn’t starting her day feeling like a failure, and the whole family dynamic shifted.
The research on this stuff is solid. Studies in journals like the Journal of Family Nursing show that when behavioral therapy is started early and done consistently, it can have lasting effects. But here’s the key – it has to be consistent. You can’t do it for a few weeks and then give up when life gets busy.
Behavioral Parent Training is a huge part of this too. Parents learn specific techniques for managing challenging behaviors, creating structure at home, and supporting their kid’s emotional regulation. And honestly, this often ends up helping the whole family, not just the kid with ADHD.
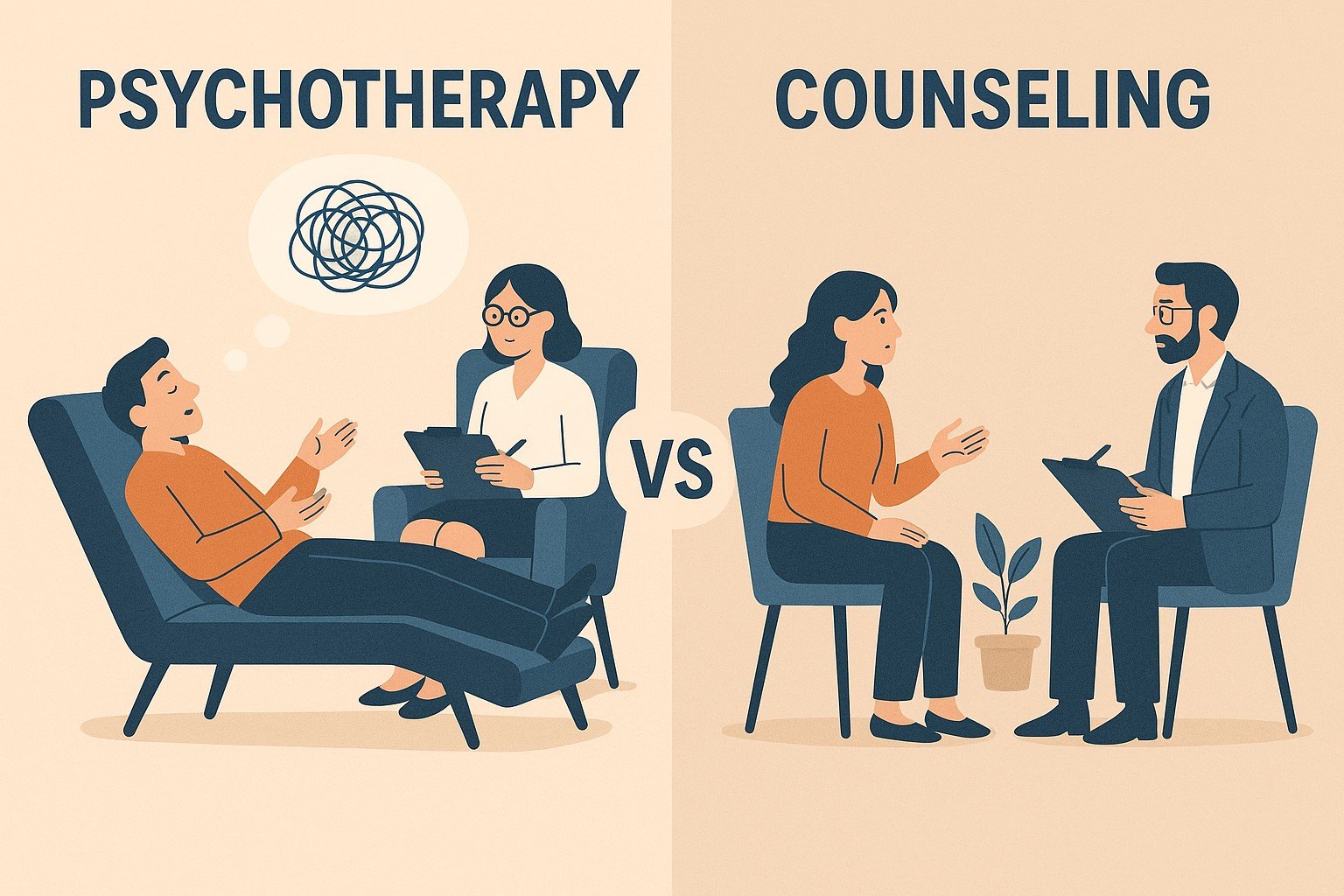
CBT for ADHD: Rewiring the Mental Patterns
For teenagers and adults (who can find additional resources at ADDA), Cognitive Behavioral Therapy is often where we see the biggest breakthroughs. CBT for ADHD is all about identifying those unhelpful thought patterns that keep you stuck and learning practical strategies for managing focus, planning, and emotions.
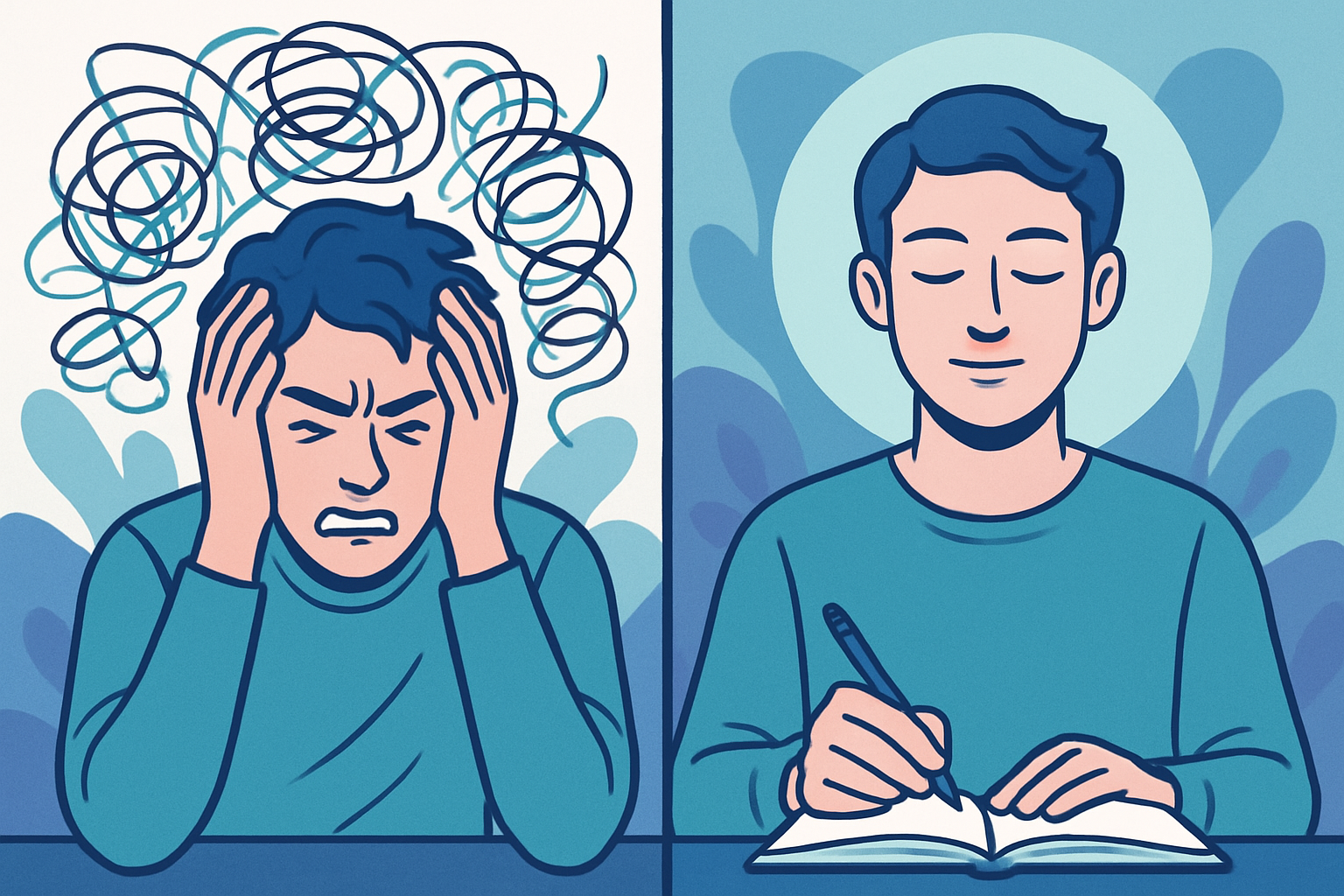
Here’s what I love about CBT – it addresses not just the ADHD symptoms themselves, but all the secondary stuff that builds up over years of struggling. The low self-esteem, the anxiety about forgetting things, the depression that can come from feeling like you’re constantly failing at “simple” tasks.
I had this client, Sarah (different Sarah from before), who was a marketing professional in her late twenties. She came to me feeling completely overwhelmed and convinced she was just lazy and incompetent. She was missing deadlines, forgetting meetings, and had this constant internal dialogue of “Why can’t I just get it together like everyone else?”
Through CBT, we started unpacking those thoughts. Turns out, a lot of her procrastination wasn’t about laziness at all – it was about perfectionism and fear of failure. She’d rather not start something than risk doing it poorly. Once we identified that pattern, we could work on breaking big projects into smaller pieces, setting realistic deadlines, and celebrating progress instead of waiting for perfection.
The transformation was pretty amazing. Within about six months, she’d gotten a promotion at work. But more importantly, she’d developed a much healthier relationship with herself and her ADHD.
The research on CBT for ADHD is really strong. Studies by researchers like Newark and Stieglitz show significant improvements in executive functioning – things like time management, task initiation, and dealing with frustration. And it tends to work even better when it’s combined with other approaches like coaching or medication.
ADHD Coaching: The Practical Stuff That Actually Matters
Now, this is where I get excited because coaching is what I do, and I’ve seen it change people’s lives. ADHD coaching is different from traditional therapy because we’re not really digging into your childhood or processing trauma (though that stuff can be important too). We’re focused on the here and now – what systems do you need to function better in your daily life?
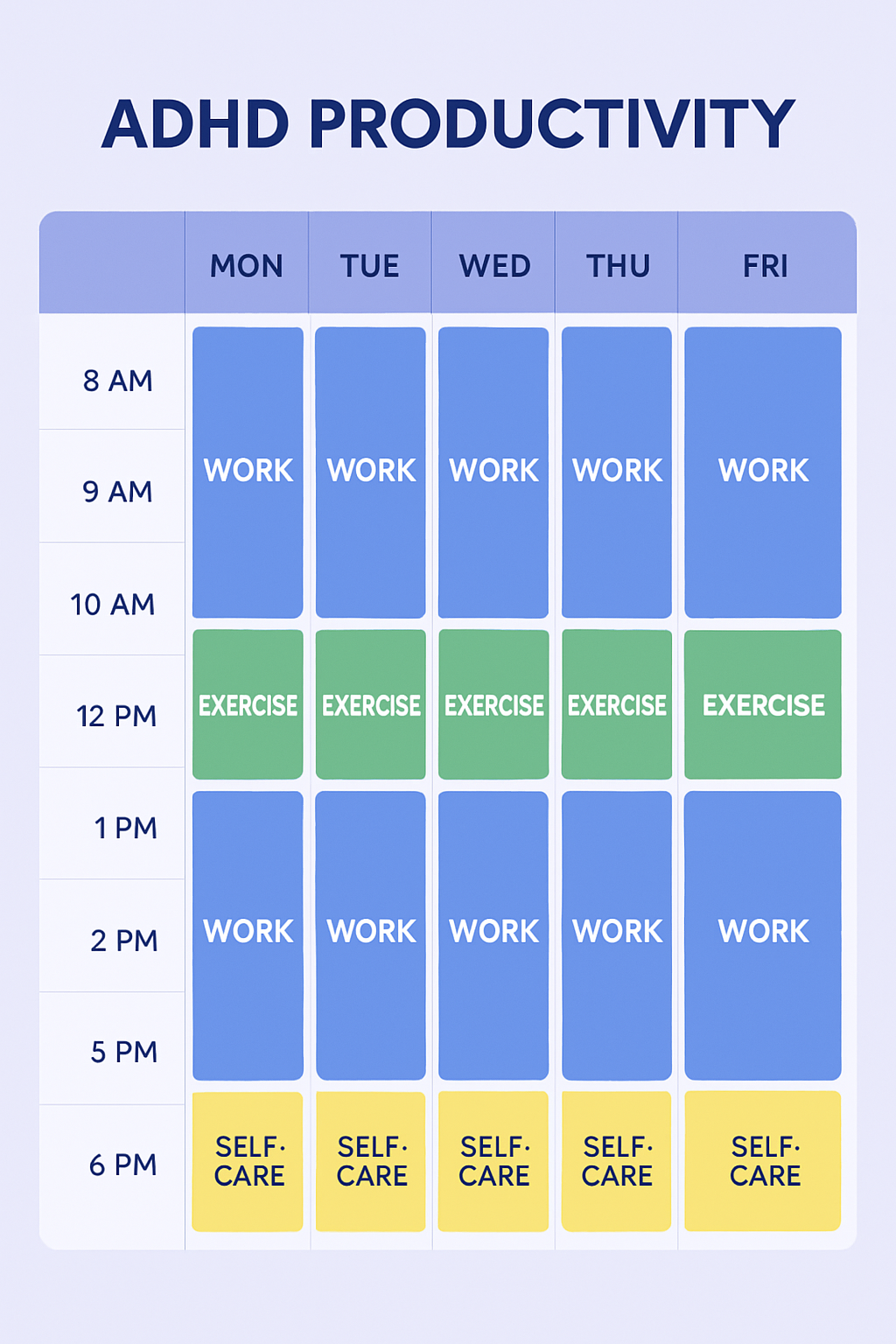
Coaching is all about working WITH your ADHD brain instead of against it. We figure out your natural strengths and build systems that leverage those strengths rather than trying to force you into neurotypical productivity methods.
I had this client, Marcus, who’s a software developer. He was constantly missing deadlines and felt like he was always behind on projects. Traditional time management advice made him feel worse because it was all about steady, consistent effort throughout the day. But Marcus’s brain doesn’t work that way – he works best in intense, focused bursts.
So we created what we called a “sprint and recovery” system. He’d work intensely for 90-minute blocks, then take a 30-minute break to move around or do something completely different. We set up visual project tracking so he could see his progress, and we built in buffer time for the inevitable hyperfocus sessions where he’d work for six hours straight and forget to eat.
The difference was night and day. Not only did he start meeting deadlines consistently, but his work quality improved because he was working with his brain’s natural patterns instead of fighting them.

At our practice, Heal and Thrive Psychotherapy and Coaching, we use a strength-based, neuroscience-informed approach to coaching. We understand that ADHD brains are wired differently, and we use that knowledge to create strategies that actually work in real life.
Coaching often works really well combined with other approaches. Maybe you’re doing CBT to work on thought patterns while also doing coaching to build practical systems. Or you might be on medication that helps with focus while using coaching to develop organizational skills.
Mindfulness and DBT: When Emotions Feel Out of Control
Okay, I’ll be honest – when I first heard about using mindfulness for ADHD, I was skeptical. I mean, telling someone with ADHD to sit still and focus on their breath? That sounds like torture, right?
But it turns out, when mindfulness is adapted for ADHD brains, it can be incredibly helpful. We’re not talking about traditional meditation where you sit cross-legged for an hour. We’re talking about practical mindfulness techniques that help with attention, impulse control, and emotional regulation.
The research on mindfulness is actually pretty cool. Regular mindfulness practice literally changes how attention networks function in the brain. It can help reduce stress, which we know makes ADHD symptoms worse. And it builds self-awareness, which is crucial for managing ADHD effectively.
For people with ADHD, we might use walking meditation, body-based awareness practices, or mindfulness activities that incorporate movement. The key is finding approaches that work with ADHD symptoms rather than against them.
DBT – Dialectical Behavior Therapy – has also been adapted for ADHD, especially for people who struggle with intense emotions. DBT teaches specific skills for managing overwhelming feelings, improving relationships, and tolerating distress.
I worked with a teenager, Alex, who was having explosive emotional outbursts at home and school. Traditional behavior management wasn’t working because the emotions were just too intense. Through DBT-informed techniques, Alex learned to recognize emotional triggers early, use grounding techniques when things got overwhelming, and communicate needs more effectively.
The improvement in family relationships was dramatic. Alex’s parents went from walking on eggshells to actually enjoying spending time together. And Alex’s performance at school improved because emotional meltdowns weren’t derailing the whole day anymore.

Neurofeedback: Training Your Brain Directly
For families who want to avoid medication or haven’t had success with traditional approaches, neurofeedback is an interesting option. Basically, you’re training your brain to produce more optimal brainwave patterns through real-time feedback.
The research on neurofeedback for ADHD is promising. Studies by researchers like Baumeister and Zuberer have shown improvements in attention and impulse control. It’s not a magic cure, but for some people, it can be a helpful piece of the puzzle.
The process involves putting sensors on your scalp to monitor brainwave activity, then playing computer games or watching videos that respond to your brain patterns. When your brain produces the desired patterns, you get positive feedback in the game.
What I like about neurofeedback is that it gives people a sense of agency in their treatment. Instead of being passive recipients of therapy, they’re actively learning to influence their brain function.
But I’ll be real with you – neurofeedback requires a significant time commitment, and it can be expensive. It works best as part of a comprehensive approach rather than as a standalone treatment.
The Supporting Cast: Other Approaches That Can Make a Difference
Social Skills Training: Because Relationships Matter
A lot of people with ADHD struggle with social interactions. Maybe they interrupt conversations because they’re impulsive, or they miss social cues because they’re distracted, or they have trouble maintaining friendships because they forget to follow up with people.
Social skills training provides structured practice with things like turn-taking in conversations, reading nonverbal cues, and managing conflict. For kids and teenagers especially, this can make a huge difference in their confidence and relationships.
I’ve seen kids go from being isolated and lonely to having genuine friendships after working on social skills. It’s not about changing who they are – it’s about giving them tools to navigate social situations more successfully.
Occupational Therapy: The Sensory Piece
Many people with ADHD also have sensory processing differences. Maybe they’re hypersensitive to certain textures or sounds, or maybe they need more sensory input to feel regulated. Occupational therapy can address these issues and provide tools for managing sensory challenges.
OT might involve sensory integration techniques, fine motor skill development, or environmental modifications that support focus and regulation. For kids, this might mean sensory breaks during the school day or special seating that allows for movement.
Play Therapy: For the Little Ones
Young kids often do better with play therapy than traditional talk therapy. Through play, they can process emotions, practice social skills, and develop coping strategies in a way that feels natural and fun.
Play therapy can be especially effective when combined with parent training, so there’s consistency between what’s happening in therapy and what’s happening at home.
What We Do at Heal and Thrive: A Personalized Approach
At Heal and Thrive Psychotherapy and Coaching, we don’t believe in cookie-cutter treatment plans. ADHD affects everyone differently, so treatment needs to be individualized based on your specific challenges, strengths, and goals.
We start with a comprehensive assessment to understand not just your ADHD symptoms, but your whole life context. What are your goals? What’s your environment like? What support systems do you have? What have you tried before, and how did it work?
Then we work together to create a treatment plan that might include several different approaches. Maybe we start with CBT to address some negative thought patterns, add in some coaching to build practical systems, and incorporate mindfulness techniques for emotional regulation.
Our approach is collaborative. You’re not a passive recipient of treatment – you’re an active partner in figuring out what works for you. We adjust and modify as we go based on what’s helping and what isn’t.
We also take a whole-family approach when appropriate. ADHD doesn’t just affect the person who has it – it affects the whole family system. Sometimes the most effective intervention is helping family members understand ADHD better and learn how to support each other.
When Things Don’t Go According to Plan (Because They Usually Don’t)
Let’s be honest – ADHD treatment isn’t a straight line from problem to solution. There are going to be setbacks, frustrations, and times when you feel like nothing is working.
When Progress Feels Slow
One of the most common things I hear is “I’ve been doing this for months, and I don’t feel like anything is changing.” I get it. When you’re struggling with ADHD symptoms every day, you want relief NOW.
But here’s the thing – ADHD treatment is often about building new neural pathways and habits, which takes time. The changes might be subtle at first. Maybe you’re still forgetting appointments, but you’re remembering to write them down more often. Maybe you’re still procrastinating on big projects, but you’re able to start smaller tasks more easily.
These small changes are actually signs that your brain is learning new patterns. They’re worth celebrating, even if they don’t feel dramatic.
If progress really seems stalled, it might be time to reassess. Maybe we need to try a different approach, address other factors that might be interfering (like sleep problems or stress), or adjust medication if that’s part of your treatment plan.
The Medication Question
I know a lot of people have complicated feelings about ADHD medication. Some people worry about side effects, others feel like medication isn’t enough on its own, and some prefer to try non-medication approaches first.
All of these perspectives are valid. There’s no “right” answer about medication – it’s a personal decision that should be made based on your specific situation and in consultation with a healthcare provider who understands ADHD.
What I can tell you is that the most effective ADHD treatment usually involves multiple approaches. Medication can provide a foundation that makes other interventions more effective, but it’s rarely a complete solution on its own. Therapy, coaching, lifestyle changes, and skill-building remain important regardless of whether medication is part of your plan.
Dealing with Setbacks
ADHD symptoms can fluctuate based on stress, life changes, hormonal shifts, and other factors. It’s completely normal to have periods where symptoms feel more challenging, even when you’ve been doing well.
I always prepare my clients for this because setbacks can feel really discouraging if you’re not expecting them. But a setback doesn’t mean your previous progress was meaningless or that treatment isn’t working. It usually means you need to adjust your strategies, increase support, or address new stressors in your life.
Family Dynamics
ADHD affects the whole family, and sometimes family members have different opinions about treatment or struggle to understand and support the person with ADHD. These dynamics can significantly impact treatment success.
Family therapy or family education can be incredibly helpful in these situations. When everyone understands ADHD and learns how to support each other effectively, the whole family benefits.
How Do You Know If It’s Working?
This is such an important question because ADHD symptoms can be subjective, and progress isn’t always obvious or linear.
Look for Functional Improvements
The most meaningful measure of success is how well you’re able to manage daily life. Are you meeting deadlines more consistently? Are your relationships improving? Do you feel less overwhelmed by everyday tasks? Are you feeling better about yourself?
For kids, this might look like better performance at school, improved behavior at home, stronger friendships, or increased independence with daily routines.
Don’t Expect Perfection
The goal isn’t to eliminate all ADHD symptoms – that’s often neither realistic nor necessary. The goal is to reduce symptoms to a level where they don’t significantly interfere with your daily functioning and quality of life.
Consider the Whole Picture
Successful ADHD treatment should improve your overall quality of life. This includes things like stress levels, sleep quality, relationship satisfaction, work or school performance, and general life satisfaction.
Think Long-Term
Good ADHD treatment gives you tools and strategies that you can use throughout your life. It helps you develop self-awareness about your ADHD, learn effective coping strategies, build supportive relationships, and know when and how to seek additional help when needed.
Ready to Take the Next Step?
Look, living with ADHD can be challenging, but it doesn’t have to define your limits. Whether you’re dealing with focus issues, struggling with impulsivity, feeling frustrated with approaches that haven’t worked, or supporting someone you love with ADHD, there are effective treatments out there.
The key is finding an approach that’s personalized to your specific needs and based on solid research. At Heal and Thrive Psychotherapy and Coaching, we believe that everyone with ADHD has the potential to thrive – not despite their diagnosis, but because of the unique strengths that often come with ADHD thinking.
With the right support, tools, and strategies – whether that’s CBT, coaching, behavioral therapy, mindfulness training, or a combination of approaches – you can make real progress toward feeling more confident, capable, and in control of your daily life.
If you’re ready to explore what might work for you, we’d love to help. You can contact our ADHD specialists for a free consultation to talk through your options or book a session with one of our therapists or coaches to get started.
You don’t have to figure this out alone. Let’s work together to find what works for you.