What Is the Most Effective Mental Health Treatment?
I remember a client, I’ll call her Sarah, who walked into my office after years of trying “everything.” And by everything, I mean medication, meditation, talk therapy, journaling, yoga retreats, self-help books (a whole shelf of them), and even a wellness app that tracked her moods by color.
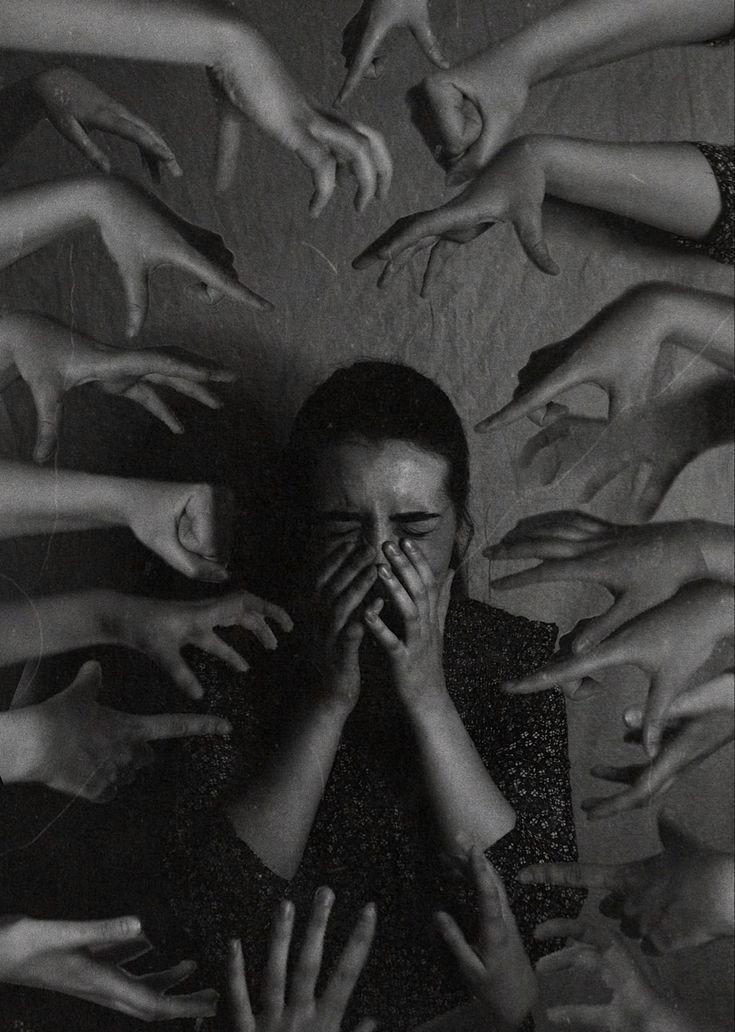
She was exhausted.
Frustrated.
And, if I’m being completely honest, skeptical that I could offer her anything different.
“Just tell me what works,” she said. “Like, what’s the best treatment for anxiety and depression? Is there even one that really works?”
Now that’s the million-dollar question, right?
And truthfully… the answer isn’t as simple as we’d like it to be. But here’s the good news: we do know what works best, most of the time, for most people. Not perfectly. Not immediately. But predictably. That’s where evidence-based therapy comes in.
So, let’s break this down together—step by step—because if you’ve ever asked, “What’s the most effective mental health treatment?” or “How do I find the best therapist near me?” … you’re in exactly the right place.
Why We Even Ask This Question
Because let’s face it, mental health treatment isn’t like treating a broken bone. There’s no one-size-fits-all cast for depression or anxiety. And if you’ve ever tried something that “worked wonders” for someone else, only to feel nothing, you already know that frustrating truth.
The Real Problem We’re All Facing
- One therapy doesn’t work for everyone.
Your brain is different. Your history is different. Your environment, your stressors, your trauma, all unique.
- There’s too much information, not enough clarity.
Do you need CBT? EMDR? DBT? Meds? Meditation? And wait, what even is a “mental health counselor” vs. a “therapist” vs. a “coach”?
- Access is wildly unequal.
In rural areas of California? Good luck getting weekly in-person therapy without a 3-month waitlist. And let’s not even start on costs.
- And stigma? Still real.
Even in 2025, many still feel judged for needing support. This silence is costing lives.
So yeah… the question “What’s the most effective mental health treatment?” isn’t just curiosity, it’s about survival, hope, and clarity in the middle of confusion.
Quick Answer:
The most effective mental health treatments tend to be evidence-based, tailored to the individual, and often combine therapy + lifestyle + sometimes medication.
But the real answer? Let’s get into the details.
What Actually Works for Real People
(Because research is great, but so are human experiences.)
Let me tell you about Jamal (not his real name, of course).
Jamal was a 29-year-old graphic designer from Oakland, California. On paper? Talented, hardworking, hilarious in that dry, sarcastic kind of way.
But behind the scenes, Jamal was quietly drowning in what he described as “a fog I can’t get out of.” He’d been to three different therapists over the years—none of whom felt like the right fit. He’d tried Zoloft, Lexapro, even St. John’s Wort (because hey, TikTok said it worked).
By the time he found me, he was almost done trying.
We started with a full evaluation. Not just symptoms, but patterns, his sleep, energy, social withdrawal, even his perfectionism. What we discovered was that Jamal didn’t just have depression. He was also living with undiagnosed ADHD, which explained a lot about his procrastination, low self-esteem, and inability to stick with any treatment plan.
What Worked for Jamal?
A combination of:
- CBT (Cognitive Behavioral Therapy) tailored to both depression and ADHD.
- Medication adjusted after a psychiatrist reviewed his full picture.
- Daily routines + accountability tools, like a simple app with reminders (not 10 apps, just one that actually worked for him).
- Weekly therapy focused on breaking shame cycles and building self-compassion.
Within four months? Not cured. But better. Jamal was functioning. He laughed again. And he kept going.

But Why Does This Matter?
Because Jamal’s story is not unusual.
Many people cycle through treatments that don’t work, not because the treatments are bad, but because they aren’t matched to the person. That’s the core message here:
The most effective mental health treatment is the one that fits the individual’s needs, diagnosis, biology, and life context.
Let’s look at another example, Maria, a 42-year-old mother of three in Fresno.
Her anxiety didn’t respond well to traditional talk therapy. What finally helped?
- EMDR (Eye Movement Desensitization and Reprocessing) for past trauma.
- Breathwork and grounding exercises she could do while parenting.
- A local women’s therapy group that gave her emotional safety and validation she’d never had before.
It wasn’t fast. But it was real.
A Quick Note from Me to You
If you’ve tried something and it didn’t work, please hear this:
It doesn’t mean therapy doesn’t work.
It just means that approach didn’t work for you.
And that’s okay. You’re not broken. You just haven’t found the right fit, yet.
What Actually Works?
Practical, Evidence-Based Mental Health Treatments That Get Results
Okay, deep breath. Let’s get into what actually works, and why.
Because here’s the thing: mental health treatment isn’t about guessing. Not anymore.
Decades of research, thousands of studies, and millions of client hours have helped us learn what consistently brings people relief. It’s not always perfect, but it’s better than hoping and wishing.
Let’s break it down into categories, based on both clinical research and real-world outcomes.
- Cognitive Behavioral Therapy (CBT)
One of the most widely studied and supported treatments for depression and anxiety.
CBT helps people identify and change negative thought patterns. But here’s what most people miss: it’s not just about “positive thinking.” It’s a structured, problem-solving method that teaches clients to examine evidence behind their thoughts.
Why It Works:
- It’s short-term (usually 12–20 sessions).
- It’s skills-based (clients actually learn tools).
- Research shows it’s as effective as medication for mild to moderate depression (Elkin et al., 1989).
Client Insight:
I had a client, let’s call her Dana, who had paralyzing anxiety about work. We used CBT to map her thought distortions (like “If I make a mistake, I’ll get fired”), and slowly, her panic attacks reduced from weekly to occasional nerves. She even started mentoring others at work, something unthinkable before.
- Medication (When Appropriate)
SSRIs, SNRIs, mood stabilizers, these can be life-changing, especially when symptoms are severe.
But let me be clear: meds aren’t magic. They’re tools. They help level the playing field so therapy can actually work.
What to Watch For:
- Side effects (e.g., weight changes, libido issues)
- Misdiagnosis (e.g., treating bipolar depression with SSRIs alone can worsen symptoms)
- Trial and error—sometimes it takes 2–3 tries to find the right fit
What the Research Says:
Combining meds + therapy is more effective than either alone in many cases (Andrews, 1999).
- EMDR (Eye Movement Desensitization and Reprocessing)
Originally for trauma, now widely used for anxiety, phobias, even chronic pain.
This therapy may sound strange (think: following a finger back and forth while recalling traumatic memories), but it’s grounded in neuroscience. EMDR helps the brain reprocess stuck emotional memories so they lose their sting.
Clients often say: “I still remember the trauma, but it doesn’t control me anymore.”
- Mindfulness-Based Therapies
MBSR, ACT, MBCT, all blend mindfulness with psychological techniques.
These methods are perfect for clients who struggle with rumination, perfectionism, or chronic stress. Instead of changing thoughts, mindfulness helps you observe them without getting hooked.
Example: One client of mine used body scans before meetings to manage panic attacks, an ACT technique that helped her stay grounded.
- Lifestyle & Behavioral Interventions
Sleep. Diet. Exercise. Social connection.
They sound simple… but they’re powerful.
For some clients, a 30-minute walk every morning does more than any pill they’ve tried. Others find relief from tracking sleep patterns and reducing sugar/caffeine.
These aren’t “replacements” for therapy. They’re foundations that support it.
- Group Therapy & Support Groups
Connection reduces shame. Community improves outcomes.
Sometimes, just hearing “me too” changes everything.
Group settings offer validation, accountability, and cost-effective access to care. Especially for trauma survivors and people managing chronic conditions like bipolar or OCD.
- New & Emerging Treatments
TMS (Transcranial Magnetic Stimulation), Ketamine-Assisted Therapy, and Psychedelic-Assisted Psychotherapy
Promising, but not a silver bullet.
While these cutting-edge approaches are exciting, we’re still learning about long-term effects. They’re expensive, not always covered by insurance, and need strict medical supervision.
That said? I’ve had clients who found real relief from ketamine infusions, after trying years of other options.
Pro Tip: No single treatment works for everyone—but almost everyone benefits from a tailored combination.
Real People, Real Progress
Stories That Show How Mental Health Treatment Can Change Lives
Let’s be honest, clinical data is great, but human stories are what bring the science to life.
Here are a few anonymized stories (names changed) from my therapy room that show how different approaches help real people with real challenges.
Jamila – Panic to Public Speaking
The Challenge:
Jamila, 28, avoided elevators, meetings, and dating.
She’d had multiple panic attacks in college, and ever since, she structured her whole life to avoid anything that could trigger anxiety.
The Approach:
We used a mix of CBT, exposure therapy, and breath retraining.
She learned how to challenge her catastrophic thoughts and gradually re-enter situations she once feared.
The Result:
Nine months later, she gave a presentation at work on the 10th floor, something she never thought possible.
Jamila said: “I still get nervous, but it doesn’t rule me anymore. I finally feel like me again.”
Kevin – Depression and the Dopamine Trap
The Challenge:
Kevin, a 35-year-old graphic designer, described “waking up sad and scrolling ‘til I’m numb.”
He was stuck in a loop of doomscrolling, video games, skipped meals, and missed deadlines. He also slept 12+ hours a day.
The Approach:
We started with behavioral activation, getting him moving before his brain “wanted” to.
Eventually we layered in sleep hygiene, nutrition tracking, and short-form CBT modules online.
His psychiatrist also started him on an SSRI.
The Result:
He slowly got back into his creative flow. His sleep regulated. He got promoted within a year.
Kevin said: “It wasn’t one thing, it was the combo that saved me. I didn’t even realize how far I’d spiraled until I started climbing out.”
Maria – Breaking Generational Cycles
The Challenge:
Maria, a 43-year-old single mother, came to therapy exhausted. She was repeating the same explosive parenting patterns she grew up with, and she hated it.
The Approach:
We explored her childhood trauma, introduced EMDR, and taught gentle parenting tools.
She also joined a trauma-informed group for moms.
The Result:
Six months later, her daughter said, “Mom, you don’t yell like before.” Maria cried in session.
Maria said: “I thought therapy was for rich people. Turns out, it’s for anyone who wants to break the cycle.”
Why These Stories Matter
They’re not perfect fairy tales.
Each one had setbacks, missed sessions, and hard weeks.
But they also had momentum, support, and breakthroughs. And that’s the real heart of healing.
These stories show that when people are offered the right support at the right time, change becomes not just possible, but probable.
Let’s Make Mental Health Less Mysterious
The more we understand, the better we get at healing.

Here’s the big takeaway:
Mental health isn’t magic or moral failure. It’s biology, behavior, and environment all braided together, and that means it’s treatable, step by step.
Whether you’re dealing with anxious thoughts, lingering trauma, or just feeling “off,” help exists, and you deserve it.
Therapy doesn’t have to be mysterious, cold, or inaccessible.
Our goal at Heal & Thrive is to make it warm, practical, and effective.
Ready to talk to someone? Reach out to us here.
Curious about which therapy approach fits you best?
Take our free 2-minute quiz to discover your best starting point.

